Study led by Indian American shows keto diet improves mental illness
Growing evidence suggests that psychiatric disorders may originate from metabolic deficiencies in the brain.
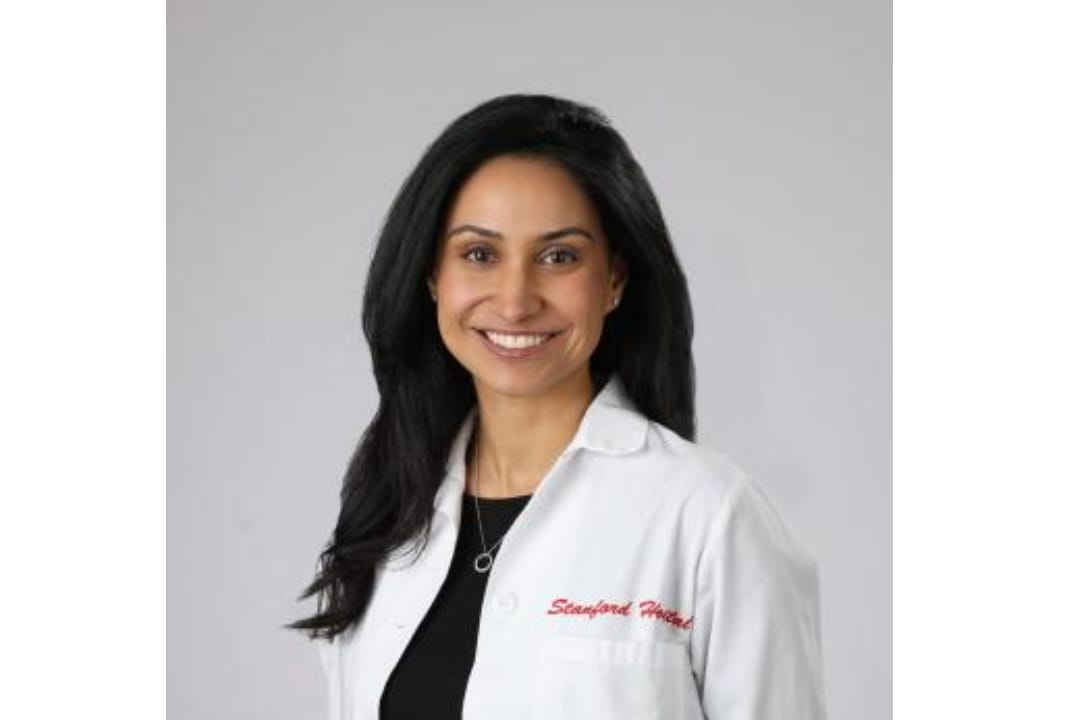 Sethi is the founder and director of the Metabolic Psychiatry Clinic at Stanford Medicine. / Image - Stanford University
Sethi is the founder and director of the Metabolic Psychiatry Clinic at Stanford Medicine. / Image - Stanford University
A pilot study conducted by researchers at Stanford Medicine led by Shebani Sethi has revealed that following a ketogenic (keto) diet can help patients deal with serious mental illness like schizophrenia or bipolar disorder.
Essentially a low-carb diet, ketogenic diets aim to deprive the body of glucose that is used to produce energy. In the absence of glucose a state of ketosis is eventually induced, during which the body turns to stored fat, which the liver converts into ketones for energy.
Published in Psychiatry Research, the findings highlight that such a diet not only reinstates metabolic health in patients who suffer from metabolic side effects due to their medications but also enhances their psychiatric conditions.
“It’s very promising and very encouraging that you can take back control of your illness in some way, aside from the usual standard of care,” said Shebani Sethi, associate professor of psychiatry and behavioral sciences and first author of the study.
“The ketogenic diet has been proven to be effective for treatment-resistant epileptic seizures by reducing the excitability of neurons in the brain. We thought it would be worth exploring this treatment in psychiatric conditions,” she added.
There is growing evidence suggesting that psychiatric disorders like schizophrenia and bipolar disorder may originate from metabolic deficiencies in the brain, which impact the excitability of neurons, Sethi explained. The researchers posit that similar to how a ketogenic diet enhances overall body metabolism, it may also positively impact brain metabolism.
“Anything that improves metabolic health in general is probably going to improve brain health anyway. But the ketogenic diet can provide ketones as an alternative fuel to glucose for a brain with energy dysfunction,” she noted.
Sethi is the founder and director of the Metabolic Psychiatry Clinic at Stanford Medicine. As a physician, she cares for many patients with both serious mental illness and obesity or metabolic syndrome. “Many of my patients suffer from both illnesses, so my desire was to see if metabolic interventions could help them. They are seeking more help. They are looking to just feel better,” she highlighted.
ADVERTISEMENT
ADVERTISEMENT
E Paper
Video




 Mehak Luthra
Mehak Luthra

.jpg)









Comments
Start the conversation
Become a member of New India Abroad to start commenting.
Sign Up Now
Already have an account? Login