Neurons have their own backup energy supply, study finds
These reserves act like emergency “backup batteries” that help neurons survive energy crises such as oxygen deprivation.
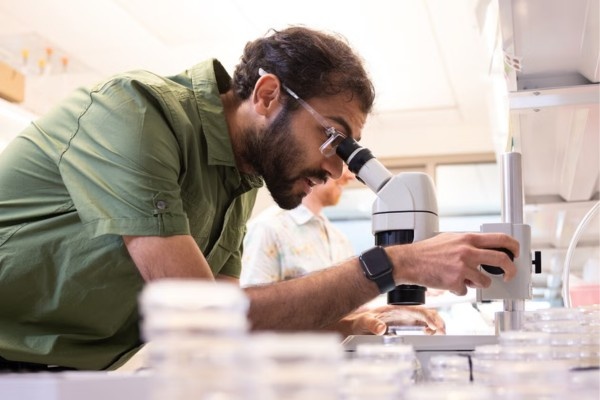 Milind Singh / Photo by Allie Barton/ Yale News
Milind Singh / Photo by Allie Barton/ Yale News
Neurons can tap into their own hidden sugar reserves to survive stress, a new study has revealed, challenging decades of assumptions about how the brain fuels itself.
The study, which was published in the Proceedings of the National Academy of Sciences, was co-led by Indian-origin researcher Milind Singh at Yale University. It reveals that neurons, long believed to depend entirely on glial (non-neuronal) cells for energy, actually possess their own glycogen stores.
Also Read: Researchers identify proteins with virus-blocking potential
These reserves act like emergency “backup batteries” that help neurons survive energy crises such as oxygen deprivation. “Traditionally, it was believed that glial cells served as ‘energy warehouses,’ storing glycogen and supplying neurons with fuel as needed,” said Singh, a fourth-year doctorate student in cell biology at Yale School of Medicine.
“But we now know that neurons themselves store glycogen and can break it down when the pressure is on. It’s like discovering your car is a hybrid — it’s been carrying an emergency battery the whole time.”
To investigate this, the team used the microscopic roundworm Caenorhabditis elegans (C. elegans) and a fluorescent biosensor called HYlight, which glows in response to changes in sugar metabolism. This allowed researchers to track neuronal energy activity in real time under varying oxygen levels.
A breakthrough came with the identification of the enzyme PYGL-1 — the worm version of the human glycogen phosphorylase enzyme. When PYGL-1 was disabled, neurons lost their ability to ramp up energy production under stress. Restoring the enzyme specifically in neurons reversed the failure, confirming that neurons themselves were activating internal reserves.
“We discovered that neurons use two different strategies to adapt to energy stress: one that’s glycogen-dependent, and one that isn’t,” said co-lead author Aaron Wolfe, a postdoctoral researcher. “The glycogen-dependent pathway is particularly critical when the mitochondria — one of the cell’s primary energy producers — aren’t functioning well.”
The researchers introduced the term “glycogen-dependent glycolytic plasticity” (GDGP) to describe this adaptive mechanism. GDGP becomes especially important during hypoxia—when oxygen supply is limited—and in diseases like stroke, epilepsy, and Alzheimer’s, where energy failure is a core problem.
“This research reshapes our understanding of brain energy metabolism and opens new avenues for exploring how to protect and support neuronal function in disease,” said senior author Dr. Daniel Colón-Ramos, professor of neuroscience and cell biology at Yale.
The study was supported by the U.S. National Institutes of Health (NIH). Recent efforts to cut reimbursements for federally funded research facilities have raised concerns about the future of similar high-impact projects.
ADVERTISEMENT
ADVERTISEMENT
E Paper
Video




 Malvika Choudhary
Malvika Choudhary











Comments
Start the conversation
Become a member of New India Abroad to start commenting.
Sign Up Now
Already have an account? Login